

Antimicrobial resistance (AMR) occurs when microorganisms such as bacteria, viruses, fungi or parasites develop the ability to survive or grow despite the presence of antimicrobial agents and antibiotics that would normally kill or inhibit them.

Antimicrobial resistance (AMR) affects health, the economy, society, and the environment. According to the World Health Organization (WHO), AMR threatens the treatment of infections caused by bacteria, viruses, fungi, and parasites. Resistant infections tend to last longer, be more severe, and spread more easily. AMR also jeopardizes medical procedures such as surgery, chemotherapy, and organ transplants, which rely on effective antimicrobials.

AMR is recognized by WHO as a major global health crisis, responsible for an estimated 4.95 million deaths in 2019, making it the third leading cause of death worldwide. Without urgent action, it could claim up to 10 million lives annually by 2050. Resistant infections also drive higher healthcare costs due to longer hospital stays, intensive care, and expensive treatments, and reduce productivity because of prolonged illness.

Beyond health, AMR threatens global economic stability. If unchecked, it could cause a cumulative loss of up to US $100 trillion by 2050. AMR affects humans, animals, plants, and the environment, highlighting the interconnectedness emphasized in the ‘One Health’ framework. Resistant microbes can spread through soil, water, and food chains, linking hospitals, farms, and natural habitats. Antimicrobial use in agriculture can fuel resistance that reaches humans and reduces food security through lower productivity and safety concerns.
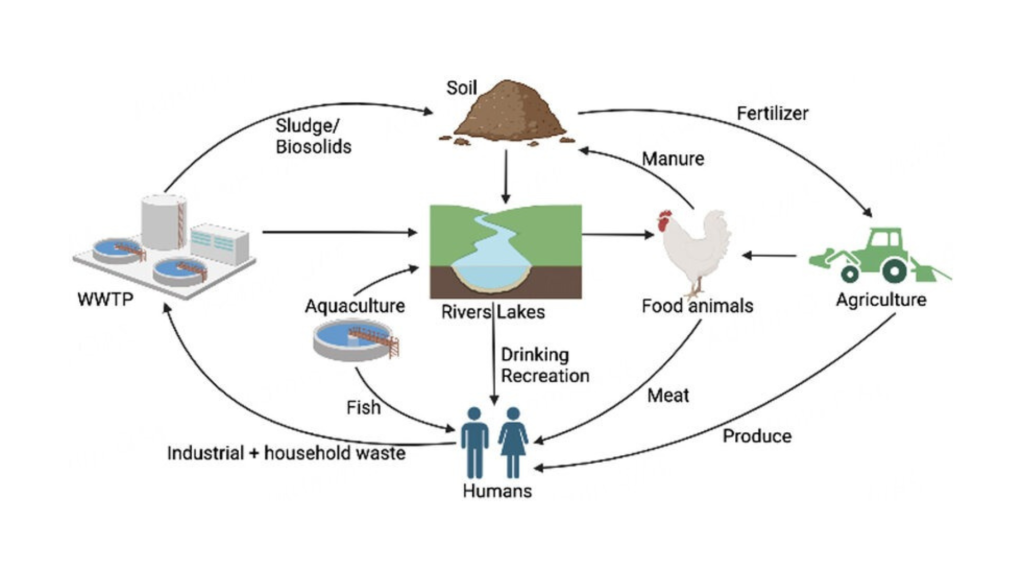
Resistant microbes in the environment pose a growing challenge. They can persist in soil and water, spreading resistance genes across microbial communities. This environmental reservoir contributes to the global propagation of AMR and underscores the importance of coordinated efforts across human, animal, and environmental health sectors.

We should care about antimicrobial resistance (AMR) because it threatens our health, wellbeing, and future.
When antimicrobials stop working, common infections become harder to treat, illnesses last longer, and diseases spread more easily. This disrupts healthcare systems, weakens the economy, and affects society as a whole. AMR impacts people, animals, plants, and the environment we all depend on.
AMR is not just a clinical or hospital problem; it’s a global concern.